Jane: My guest today is Jasmine Farrish. Jasmine is a six-year resident of Tyler, Texas, having relocated to begin Nurse Family Partnership, an evidence-based program with UT Health. The site was begun in 2016 because at that time, Smith County had the second highest poor outcomes in maternal health in the state of Texas. Jasmine is a certified nurse midwife with Community Wellness of Tyler.
She also advocates for pregnancy, Medicaid expansion and Alternative to Abortion funding to support Nurse Family Partnership. Jasmine is a Black woman prioritizing Black people, recognizing great disparities in health outcomes for Black people in Tyler and Smith County. Welcome, Jasmine Farrish.
Jasmine: Thank you, I’m excited to be here.
Jane: I’m so interested to hear about your work in Tyler and Smith County. Can you tell me how this all began for you?
Jasmine: I actually moved to Tyler to be a part of the start of Nurse Family Partnership at UT Health, because we got that bad report card. I’m happy to say that a new report just came out, and we are no longer on the bad list per se. I take good pride in that and in the stakeholders that we’ve engaged in trying to make this a better place to have a baby.
With that being said, there’s still work to do, right? I love to prioritize Black people, Black joy. Yes, the outcomes have gotten better, but there’s still a huge disparity amongst Black women and in particular, Black birthing people. We’ve got to still figure out what’s going on.
While others are focused on the quality of care or access to care, I want to go further. How do you feel about your care? Do you feel respected? Did you enjoy your pregnancy? And how are you enjoying being a parent?

Jane: Tell me a little bit more about that report card. Where do we stand now in the state of Texas? And then what I’d really love to know is what were the steps that got us from where we were in 2016 until now?
Jasmine: I would like to start with the steps, because it’s so exciting. Let’s just think about all the initiatives that we have, especially knowing that 50% of births in the state of Texas are Medicaid insured, so that’s where we focused our energy.
Evidence-based programs such as Nurse Family Partnership – we prioritized under-resourced families and first time moms – that really captive audience. Like, “I truly have never been pregnant and don’t know what to do.” They get home visits from pregnancy until the baby turns two years old. So really focusing on getting them off to a good start, a healthy pregnancy, healthy baby brain development.
But we don’t do that alone. So we partnered with Tyler Family Circle of Care, Dr. Porter, who we have a great relationship with, where we can communicate back and forth about moms who need additional support, taking a look at what kind of care that we need to provide them so that they have better outcomes.
And then you think about other grant-funded programs such as Healthy Start with BCFS. Think about doula programs, pregnancy testing centers – everybody had a hand. And we need to create wraparound services for clients, so that they have better outcomes. How can we do this together? That’s what we’ve really been focused on these last years.
Jane: Great. So, there are multiple factors and indicators for healthy pregnancy and infancy, it sounds like, as you dug into the experience of birthing people. Where did you find gaps?
Jasmine: I would say gaps in communication. As a home visitor, that’s my experience. When I come into a home, it’s a very intimate thing. You’re not coming to my office, I’m coming to you. And as I sit there attempting to serve you, I have to find common language and communication so that I can meet your needs and you feel comfortable enough to ask the questions that need answering.
As a home visitor, I will go back, take that to Family Circle of Care or to a clinic and communicate exactly what the client needs, because I have shared language in the medical field. And also to teach self-efficacy.
You have access, quote unquote, to me through Nurse Family Partnership for these years. But after that, you need to know how to navigate systems so that you can be successful in your care and your child’s care as well.
When we do a home visit, there are so many generations at the table. It just affects everyone. Everyone gets to learn, and then they tell a friend of a friend. So to me, I think communication is definitely key.
And then consistency. Sometimes we can bring in grant funded programs, but funding only lasts for so long, right?
And sustainability and being able to serve families. Because if I want you to eat better so that you have better outcomes with your child or with your pregnancy, but I didn’t ask you, “Do you have access to food? Do you have transportation to go get it? What’s the quality of the food? How do you even know what quality food is?” That takes time and I need to be able to sit with you and communicate.
Jane: Let’s dive into Black birthing people in particular. Their experience of health disparities is even greater than what was, at one time, dismal overall for Smith County. Why is their experience particularly precarious? What’s going on?
Jasmine: I think that’s what motivates me to serve in the capacity of a nurse midwife, because when we first heard numbers, we said, “Oh, it must be at the individual level.” The individual is choosing not to be healthy or to eat poorly or to smoke – whatever it may be.
Then, as you are working with families, you realize, oh no, it’s structural. There needs to be an overall change in how we approach people or how many gatekeepers there are to obtaining care.
We need to take it from individual behavior to what we can do to support health equity and ultimately health justice – is what we’re working towards.
Jane: I would love to hear any kind of anecdotes or examples you have from the field. What have you seen work, not work? Are there any trends or patterns in your experience?
Jasmine: The example I would like to give is that I had a client who was in a car accident and with her and her grandbaby in the car. She called me and she’s like, “We’re on our way to the hospital.” I immediately call her husband, meet them at the hospital to find out what’s going on.
Well, the client is in the back of the ER. The family’s in the waiting room, and they won’t let the family back to check on their wife. I kindly go up and ask for an update on the situation, because I could see the possibility of the husband getting upset, rightfully so, because he just wants to know his wife and his grandchild are okay.
I can just see it escalating, and I can see the storyline of an angry Black man who gets upset with the receptionist. All it would take was for the receptionist to say, “Sir, there are multiple traumas in the back. Give us about 15 minutes to find out an update on your wife so that we can provide you that peace of mind. But right now we can’t. We don’t have an update, and we can’t get back there to see her.” Talk to him like he’s a person who is worried about his wife and his grandchild and just wants to make sure that they are okay.
Jane: You’re talking about positive regard and assuming good things about people.
Jasmine: Yes. But just kind of standing back and watching the situation, I could see it being labeled as something else or could go a different way. That’s just a snippet of what I feel like Black people here in our community experience when they interact with the system.
Jane: It sounds like there’s a higher probability among Black people in that system for things to escalate or go awry.
Jasmine: It’s funny you mentioned “escalate” and “go awry,” because sometimes it can escalate to be more negative. But also, things go awry when there’s not enough attention or you’re not listening to people. Then, it starts a cascade of problems, and that’s how we end up dying.
Maybe we’ve said something and are not listened to, or we’re so exhausted from speaking up and not being heard that we choose not to say anything. Both can be true. That’s why I try to educate people on language to use so that you will not be dismissed.
In the maternal health world, if someone comes into your office and says, “Jas, I’m having the worst headache of my life,” those are key words we know, right? That is an emergency; we are worried about your blood pressure; worried about preeclampsia and that you need care right away.
But if you don’t have that language and you go in and say, “I have a headache,” you may get dismissed. They may assume your pain isn’t real. They may think you’re a drama queen or you’re over exaggerating or you’re seeking drugs.
All those are experiences of Black people all the time.

If you think about slavery, you’re inflicting pain on us, but we are resilient, right? We’ve dramatized this term resilient when we should not have to be resilient. Systems should be put in place so that we can just be. I think it’s interesting to be aware of your biases and to really reflect on your practices and how you interact with others. I think that’s what people are asking for.
Now that you know, what will you do? How will you reflect and change how you interact with me as a Black woman when you’re my child’s teacher at school? Can I have peace knowing when I drop my child off that you will treat them with respect?
We know that race is a construct: I bleed just like you bleed. Can I trust you when I drop my child off that you’ll treat him like the brilliant student he is and give him whatever he needs?
Those are things that we’re talking about in our community.
Jane: Tell me more about the Community Wellness Center. Where is it located? How long has it been up and running? I think you recently had an open house.
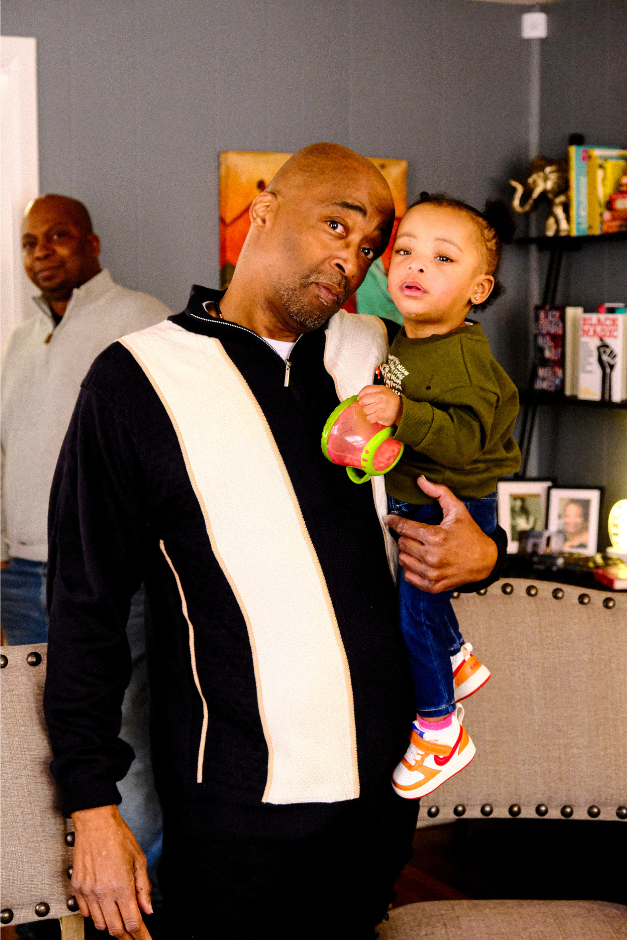
Jasmine: Yes, we were excited about our open house. Community Wellness of Tyler is on Bonner and Front streets, right in between Front and Houston, in that neighborhood. A nice little blue house on the corner. I loved our open house in February. It was called Black Birth Matters Tyler. So, just sharing a little bit about statistics in the Black community with people in the community.
They weren’t even aware of the numbers. Everybody that attended went through a supportive pregnancy group. We love group care, group support, and so you’re partnered with people that are around the same gestational age as you. You can walk through pregnancy together, hopefully building relationships and support, and so that’s what we did.
It was so great to see everybody interact, meet new people, see old friends, and we just kind of talked about whatever they wanted to talk about. We provided a tour of the facility.
Right now, we’re operating more like a medical home where people come in. They can have a one-on-one session with the midwife or they can join group sessions. Topics of groups vary from mental health, hypertension, diabetes, menopause. Our groups are phenomenal. I encourage everyone to join a group. The group is where the magic happens.
What I hear a lot from my moms is that we like options. Like, what if I didn’t want to go to the hospital, but I don’t want to initially go deliver at home either? Where’s that middle ground? So, that’s why the ultimate goal is the birthing center.
We need allocated funding to do that. We need a budget line. We need good attitudes.
I know it’s the East Texas way to be polite. I don’t want to hurt anybody’s feelings; I might have to loop around to them at another time in my life, and I want that relationship to be positive.
However, because we are being dishonest, we have bad outcomes. I can use my relationship with Dr. Josie Porter, for example. If I was afraid to collaborate with Dr. Porter or to be honest about the need to collaborate, then families wouldn’t get what they need.
Jane: What would it take for Community Wellness of Tyler to realize this dream you have of becoming a birthing center?
Jasmine: Going back to the made up system of money? Yes, funding.
Right now, we have two exam rooms or two private rooms to talk in. And then we have two group spaces, but we’ll need more space. Going back to Medicaid expansion, I don’t want the last time I see moms or people to be when six weeks postpartum is complete There’s so much that happens after six weeks postpartum. Right now, those two things are at the forefront of my mind: funding and Medicaid expansion.
Jane: What’s your great hope for Tyler and East Texas?
Jasmine: My great hope is that we remain hopeful; that we don’t lose our steam at improving our outcome; that we treat people like people; and that we become more diverse. Not only at work but in our personal circles as well, where we spend the most time.
Jane: Going back to something you said near the beginning: you talked about Black joy. I would love to hear more about that as you have your hopes for Tyler and East Texas. What is Black joy and what does it look like here?
Jasmine: Man, we’re trying to figure that out. Joy looks different for everybody. I think a lot of times, Black people feel like others may assume that there’s a single Black voice. So Black joy looks different for everybody,
Sometimes, it’s that I make it through pregnancy. Or that I am able to feed my family. I’m able to send my kids to college. You know, we find joy in anything.
A lot of times I feel that Tyler centers the white male experience. And so, I would like to diversify that.
Jane: What got you into this line of work? Is there anything personal that you want to share with us?
Jasmine: So, I was a labor and delivery nurse right out of undergraduate school, and I had a young teenage mom. She was maybe 13, 14.
Jane: That’s young.
Jasmine: That’s very young. So, she has a vaginal birth with fourth degree lacerations, meaning, as my grandmother would say, “from the ruda to the tuda” – from the vaginal area to her bottom. And the provider only wrote Motrin for pain management. And she’s in so much pain that she’s crying, asking for help.
I’m like, “Okay, I need to get an order from the doctor for additional pain management.” When I come in contact with the doctor, he says, “Well, I bet she won’t do that again. She doesn’t need anything additional. This will be her lesson learned.”
And that’s unacceptable. It’s unacceptable. That was my personal charge to figure out what I need to do to provide better care. That story’s always my “why” in my practice.
No one should ever feel that way. Everyone should be heard. Nobody should be crying out for help in a room full of people. And providers are not there to teach us lessons. They’re there to listen to us, to provide appropriate care according to evidence-based research. So yeah, that is my “why.” Thank you for asking.
Jane: Jasmine Farrish, it’s a pleasure having you. Thank you for sharing with The Tyler Loop.
Jasmine: Oh, thank you for having me. I enjoy you. I find it a privilege to be here.
Love what you're seeing in our posts? Help power our local, nonprofit journalism platform — from in-depth reads, to freelance training, to COVID Stories videos, to intimate portraits of East Texans through storytelling.
Our readers have told us they want to better understand this place we all call home, from Tyler's north-south divide to our city's changing demographics. What systemic issues need attention? What are are greatest concerns and hopes? What matters most to Tylerites and East Texans?
Help us create more informed, more connected, more engaged Tyler. Help us continue providing no paywall, free access posts. Become a member today. Your $15/month contribution drives our work.